New AI model using socialmediaposts may help predict community deaths from opioiduse stonybrooku NaturePortfolio
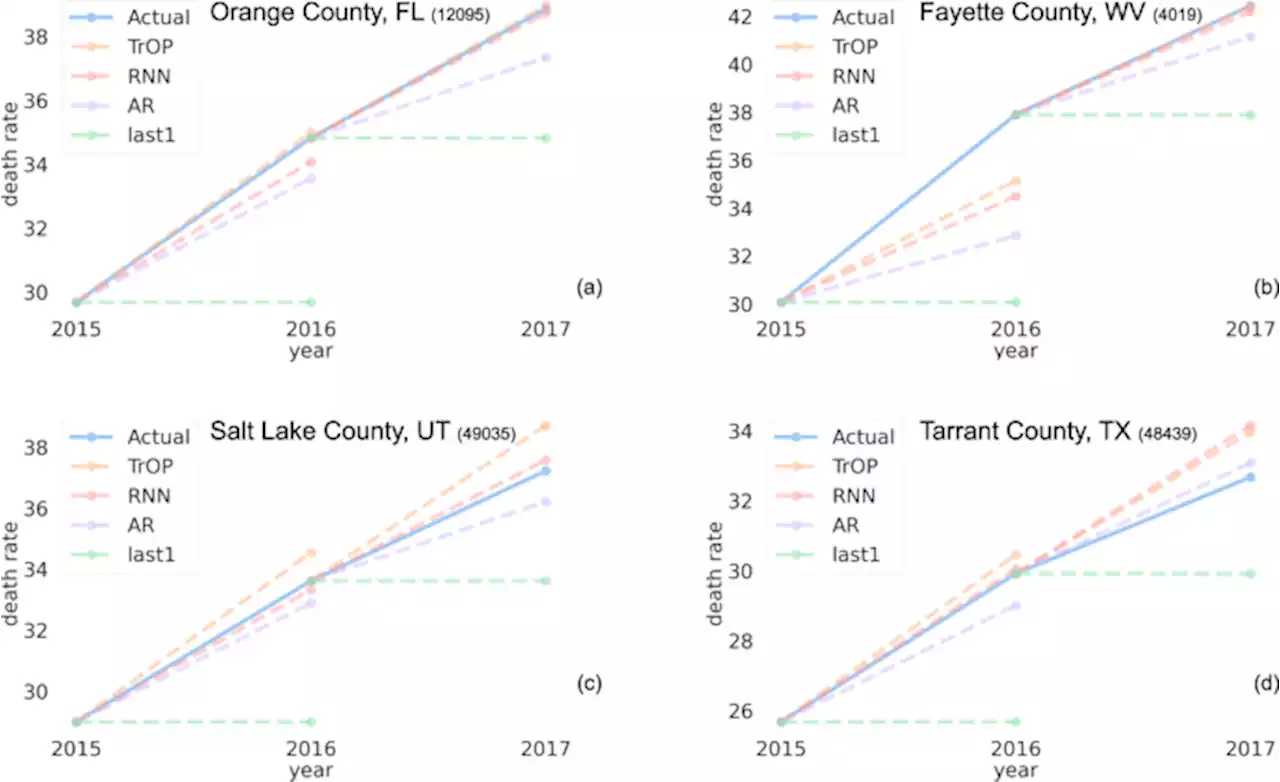
. Overall we found that each model’s error was mostly stable over both years, but did see a clear trend in 2016 being a harder year to forecast.Mean absolute error and 95% confidence intervals across our 2 test years for each statistical model. TOP appeared to be in having a more robust prediction of 2016, with a reduction of 0.6 MAE when compared to RNN. However, all models followed the same trend of 2016 being a bit harder to predict than 2017.
with a 95% confidence interval. In general, we saw a decrease in error as the number of tweets increases with the effects tailing off at 160,000 tweets.Impact of the number of tweets on error, as measured by deaths per 100k, per county for the test year . The line on the graph is fit with a LOWESS regressionOP shows a trend of decreasing error as counties have increasingly more language to build topic representations from.
We investigated the utility of such an approach by comparing our model’s performance using only a univariate input versus a multivariate one; as shown in Table. Here, we found that all models saw a considerable drop in predictive power when the language features were removed. These results highlight how each model benefited from the inclusion of language-based features from Twitter. Some models, such as the linear autoregressive ridge saw only a small increase in error, 0.
Table 3 Comparison of performance across all of our proposed machine learning models in a univariate context and their ideal history length in the number of years they have access to.To gain insight into the individual language patterns that reliably predicted future opioid deaths, we evaluated the relationship between changes in each of the topics prior to changes in the outcomes for both 2016 and 2017.
日本 最新ニュース, 日本 見出し
Similar News:他のニュース ソースから収集した、これに似たニュース記事を読むこともできます。
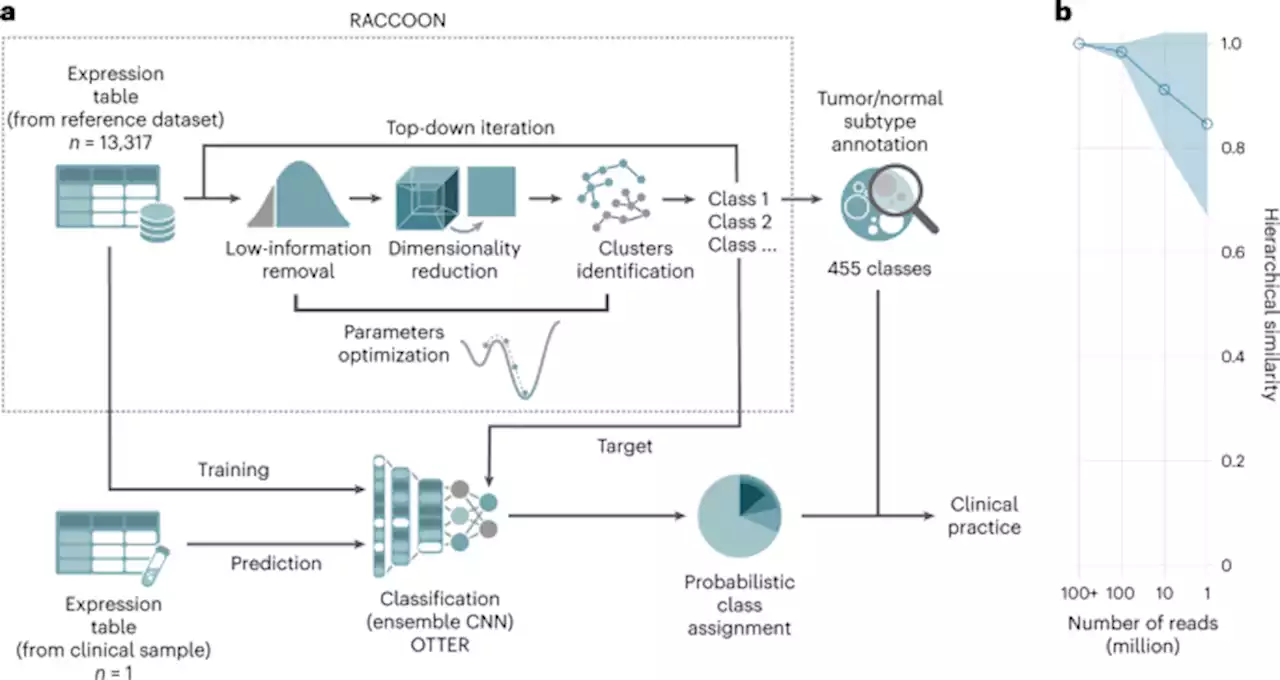 Diagnostic classification of childhood cancer using multiscale transcriptomics - Nature MedicineA new multilevel clustering approach applied retrospectively to 13,000 transcriptomes of different tumors reveals a new diagnostic classification of childhood cancers, in some cases allowing a better prediction of disease outcomes.
Diagnostic classification of childhood cancer using multiscale transcriptomics - Nature MedicineA new multilevel clustering approach applied retrospectively to 13,000 transcriptomes of different tumors reveals a new diagnostic classification of childhood cancers, in some cases allowing a better prediction of disease outcomes.
続きを読む »
 Prevalence and correlates of prescription opioid use among US adults, 2019–2020This study estimates the prevalence of prescription opioid use (POU) in the United States (US) in 2019–2020, both in the general population and specifically among adults with pain. It also identifies key geographic, demographic, and socioeconomic correlates of POU. Data were from the nationally-representative National Health Interview Survey 2019 and 2020 (N=52,617). We estimated POU prevalence in the prior 12 months among all adults (18+), adults with chronic pain (CP), and adults with high-impact chronic pain (HICP). Modified Poisson regression models estimated POU patterns across covariates. We found POU prevalence of 11.9% (95% CI 11.5, 12.3) in the general population, 29.3% (95% CI 28.2, 30.4) among those with CP, and 41.2% (95% CI 39.2, 43.2) among those with HICP. Findings from fully-adjusted models include the following: In the general population, POU prevalence declined about 9% from 2019 to 2020 (PR=0.91, 95% CI 0.85, 0.96). POU varied substantially across US geographic regions: It was significantly more common in the Midwest, West, and especially the South, where adults had 40% higher POU (PR=1.40, 95% CI 1.26, 1.55) than in the Northeast. In contrast, there were no differences by rural/urban residence. In terms of individual characteristics, POU was lowest among immigrants and among the uninsured, and was highest among adults who were food insecure and/or not employed. These findings suggest that prescription opioid use remains high among American adults, especially those with pain. Geographic patterns suggest systemic differences in therapeutic regimes across regions but not rurality, while patterns across social characteristics highlight the complex, opposing effects of limited access to care and socioeconomic precarity. Against the backdrop of continuing debates about benefits and risks of opioid analgesics, this study identifies and invites further research about geographic regions and social groups with particularly high or low prescription opioid u
Prevalence and correlates of prescription opioid use among US adults, 2019–2020This study estimates the prevalence of prescription opioid use (POU) in the United States (US) in 2019–2020, both in the general population and specifically among adults with pain. It also identifies key geographic, demographic, and socioeconomic correlates of POU. Data were from the nationally-representative National Health Interview Survey 2019 and 2020 (N=52,617). We estimated POU prevalence in the prior 12 months among all adults (18+), adults with chronic pain (CP), and adults with high-impact chronic pain (HICP). Modified Poisson regression models estimated POU patterns across covariates. We found POU prevalence of 11.9% (95% CI 11.5, 12.3) in the general population, 29.3% (95% CI 28.2, 30.4) among those with CP, and 41.2% (95% CI 39.2, 43.2) among those with HICP. Findings from fully-adjusted models include the following: In the general population, POU prevalence declined about 9% from 2019 to 2020 (PR=0.91, 95% CI 0.85, 0.96). POU varied substantially across US geographic regions: It was significantly more common in the Midwest, West, and especially the South, where adults had 40% higher POU (PR=1.40, 95% CI 1.26, 1.55) than in the Northeast. In contrast, there were no differences by rural/urban residence. In terms of individual characteristics, POU was lowest among immigrants and among the uninsured, and was highest among adults who were food insecure and/or not employed. These findings suggest that prescription opioid use remains high among American adults, especially those with pain. Geographic patterns suggest systemic differences in therapeutic regimes across regions but not rurality, while patterns across social characteristics highlight the complex, opposing effects of limited access to care and socioeconomic precarity. Against the backdrop of continuing debates about benefits and risks of opioid analgesics, this study identifies and invites further research about geographic regions and social groups with particularly high or low prescription opioid u
続きを読む »
 Bayesian network modelling to identify on-ramps to childhood obesity - BMC MedicineBackground When tackling complex public health challenges such as childhood obesity, interventions focused on immediate causes, such as poor diet and physical inactivity, have had limited success, largely because upstream root causes remain unresolved. A priority is to develop new modelling frameworks to infer the causal structure of complex chronic disease networks, allowing disease “on-ramps” to be identified and targeted. Methods The system surrounding childhood obesity was modelled as a Bayesian network, using data from The Longitudinal Study of Australian Children. The existence and directions of the dependencies between factors represent possible causal pathways for childhood obesity and were encoded in directed acyclic graphs (DAGs). The posterior distribution of the DAGs was estimated using the Partition Markov chain Monte Carlo. Results We have implemented structure learning for each dataset at a single time point. For each wave and cohort, socio-economic status was central to the DAGs, implying that socio-economic status drives the system regarding childhood obesity. Furthermore, the causal pathway socio-economic status and/or parental high school levels → parental body mass index (BMI) → child’s BMI existed in over 99.99% of posterior DAG samples across all waves and cohorts. For children under the age of 8 years, the most influential proximate causal factors explaining child BMI were birth weight and parents’ BMI. After age 8 years, free time activity became an important driver of obesity, while the upstream factors influencing free time activity for boys compared with girls were different. Conclusions Childhood obesity is largely a function of socio-economic status, which is manifest through numerous downstream factors. Parental high school levels entangle with socio-economic status, and hence, are on-ramp to childhood obesity. The strong and independent causal relationship between birth weight and childhood BMI suggests a biological link. Our study imp
Bayesian network modelling to identify on-ramps to childhood obesity - BMC MedicineBackground When tackling complex public health challenges such as childhood obesity, interventions focused on immediate causes, such as poor diet and physical inactivity, have had limited success, largely because upstream root causes remain unresolved. A priority is to develop new modelling frameworks to infer the causal structure of complex chronic disease networks, allowing disease “on-ramps” to be identified and targeted. Methods The system surrounding childhood obesity was modelled as a Bayesian network, using data from The Longitudinal Study of Australian Children. The existence and directions of the dependencies between factors represent possible causal pathways for childhood obesity and were encoded in directed acyclic graphs (DAGs). The posterior distribution of the DAGs was estimated using the Partition Markov chain Monte Carlo. Results We have implemented structure learning for each dataset at a single time point. For each wave and cohort, socio-economic status was central to the DAGs, implying that socio-economic status drives the system regarding childhood obesity. Furthermore, the causal pathway socio-economic status and/or parental high school levels → parental body mass index (BMI) → child’s BMI existed in over 99.99% of posterior DAG samples across all waves and cohorts. For children under the age of 8 years, the most influential proximate causal factors explaining child BMI were birth weight and parents’ BMI. After age 8 years, free time activity became an important driver of obesity, while the upstream factors influencing free time activity for boys compared with girls were different. Conclusions Childhood obesity is largely a function of socio-economic status, which is manifest through numerous downstream factors. Parental high school levels entangle with socio-economic status, and hence, are on-ramp to childhood obesity. The strong and independent causal relationship between birth weight and childhood BMI suggests a biological link. Our study imp
続きを読む »
 Post-COVID dyspnea: prevalence, predictors, and outcomes in a longitudinal, prospective cohort - BMC Pulmonary MedicineBackground The pathophysiology, evolution, and associated outcomes of post-COVID dyspnea remain unknown. The aim of this study was to determine the prevalence, severity, and predictors of dyspnea 12 months following hospitalization for COVID-19, and to describe the respiratory, cardiac, and patient-reported outcomes in patients with post-COVID dyspnea. Methods We enrolled a prospective cohort of all adult patients admitted to 2 academic hospitals in Vancouver, Canada with PCR-confirmed SARS-CoV-2 during the first wave of COVID between March and June 2020. Dyspnea was measured 3, 6, and 12 months after initial symptom onset using the University of California San Diego Shortness of Breath Questionnaire. Results A total of 76 patients were included. Clinically meaningful dyspnea (baseline score | 10 points) was present in 49% of patients at 3 months and 46% at 12 months following COVID-19. Between 3 and 12 months post-COVID-19, 24% patients had a clinically meaningful worsening in their dyspnea, 49% had no meaningful change, and 28% had a clinically meaningful improvement in their dyspnea. There was worse sleep, mood, quality of life, and frailty in patients with clinically meaningful dyspnea at 12 months post-COVID infection compared to patients without dyspnea. There was no difference in PFT findings, troponin, or BNP comparing patients with and without clinically meaningful dyspnea at 12 months. Severity of dyspnea and depressive symptoms at 3 months predicted severity of dyspnea at 12 months. Conclusions Post-COVID dyspnea is common, persistent, and negatively impacts quality of life. Mood abnormalities may play a causative role in post-COVID dyspnea in addition to potential cardiorespiratory abnormalities. Dyspnea and depression at initial follow-up predict longer-term post-COVID dyspnea, emphasizing that standardized dyspnea and mood assessment following COVID-19 may identify patients at high risk of post-COVID dyspnea and facilitating early and effective managem
Post-COVID dyspnea: prevalence, predictors, and outcomes in a longitudinal, prospective cohort - BMC Pulmonary MedicineBackground The pathophysiology, evolution, and associated outcomes of post-COVID dyspnea remain unknown. The aim of this study was to determine the prevalence, severity, and predictors of dyspnea 12 months following hospitalization for COVID-19, and to describe the respiratory, cardiac, and patient-reported outcomes in patients with post-COVID dyspnea. Methods We enrolled a prospective cohort of all adult patients admitted to 2 academic hospitals in Vancouver, Canada with PCR-confirmed SARS-CoV-2 during the first wave of COVID between March and June 2020. Dyspnea was measured 3, 6, and 12 months after initial symptom onset using the University of California San Diego Shortness of Breath Questionnaire. Results A total of 76 patients were included. Clinically meaningful dyspnea (baseline score | 10 points) was present in 49% of patients at 3 months and 46% at 12 months following COVID-19. Between 3 and 12 months post-COVID-19, 24% patients had a clinically meaningful worsening in their dyspnea, 49% had no meaningful change, and 28% had a clinically meaningful improvement in their dyspnea. There was worse sleep, mood, quality of life, and frailty in patients with clinically meaningful dyspnea at 12 months post-COVID infection compared to patients without dyspnea. There was no difference in PFT findings, troponin, or BNP comparing patients with and without clinically meaningful dyspnea at 12 months. Severity of dyspnea and depressive symptoms at 3 months predicted severity of dyspnea at 12 months. Conclusions Post-COVID dyspnea is common, persistent, and negatively impacts quality of life. Mood abnormalities may play a causative role in post-COVID dyspnea in addition to potential cardiorespiratory abnormalities. Dyspnea and depression at initial follow-up predict longer-term post-COVID dyspnea, emphasizing that standardized dyspnea and mood assessment following COVID-19 may identify patients at high risk of post-COVID dyspnea and facilitating early and effective managem
続きを読む »
 Towards artificial intelligence-based learning health system for population-level mortality prediction using electrocardiograms - npj Digital Medicinenpj Digital Medicine - Towards artificial intelligence-based learning health system for population-level mortality prediction using electrocardiograms
Towards artificial intelligence-based learning health system for population-level mortality prediction using electrocardiograms - npj Digital Medicinenpj Digital Medicine - Towards artificial intelligence-based learning health system for population-level mortality prediction using electrocardiograms
続きを読む »